Hoble chronic obstructive pulmonary disease stage 3. Chronic obstructive pulmonary disease: COPD classification, obstruction management and life expectancy. Symptoms and diagnosis.
The disease can occur at any age, even in young children, and its prognosis, without treatment, is unfortunately unfavorable. But why does it develop? How to recognize the disease at an early stage?
How does lung disease develop?
How does chronic obstructive pulmonary disease develop? The mechanism of development of this pathology can be described in stages:
If you don't want to use your first name, enter "anonymous" in the "Name" field. Other fields may be filled in or left blank as required. Information from the practice of natural healing Rene Graber. Ice tissue that changes or breaks down over time cannot regenerate and lead to life-threatening situations.
Smokers or ex-smokers are considered the most vulnerable group. The disease is the fourth most common cause of death in the world, with about five million deaths annually. These numbers are growing. In Germany, the disease is the sixth most common cause of death, with a prevalence of between one and three percent, with an average age of 45 years. AT last years however, female growth is also observed.
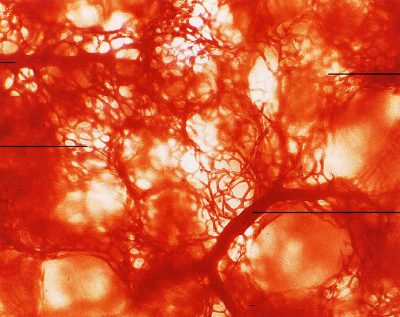
With a chronic process running, bullae appear in the lungs. What it is? This pathological process is based on the fact that when the elasticity of the bronchioles changes, they are significantly stretched. In this case, the expanded area ceases to participate in the act of breathing, provoking the occurrence of respiratory failure. With multiple bullae in patients with COPD, emphysema is diagnosed.
Symptoms and stages of COPD
Chronic bronchitis is characterized by a severe form of breathing, accompanied by mucous. Bronchial mucous membranes become irreversibly destroyed, the mucous membrane of the bronchial membrane thickens and narrows Airways. Over time, the mucosa has atrophied to such an extent that it no longer has sufficient stability. As a result, the pulmonary vesicles collapse during exhalation, and there is not sufficient ventilation. Tiny pulmonary vesicles merge with each other, their wall structure is unstable, the physiological structure of the lung is lost, and the function of obstructive emphysema develops.
It is important to know that obstructive pulmonary disease in the chronic course of the disease develops slowly.
In most cases, several years pass from the moment the mechanism of pathological changes in the bronchi is triggered under the influence of provoking factors until signs of obstruction appear. But, if obstructive changes in the bronchi have begun, this process is already irreversible, the disease will only progress and, without timely treatment, the patient will experience severe respiratory failure, which will end in death.
Besides the main cause of smoking, inhaled toxins and air pollution can also damage the lungs. This shows a clear increase in cases in densely populated residential areas, as well as adults with heavily polluted workplaces.
These include, for example, loading and hard ejection. Over time, the symptoms increase and weaken the general condition of the affected person. This leads to shortness of breath, even at rest, and continuous coughing throughout the day and during bed rest. In addition, there are signs of hypercapnia and bleeding. in the lips and nails.
Many of our readers for the treatment of cough and improvement in bronchitis, pneumonia, bronchial asthma, tuberculosis actively use the Monastic collection of Father George. It consists of 16 medicinal plants, which have an extremely high efficacy in the treatment of chronic COUGH, bronchitis and cough provoked by smoking.
It has a lean form with underdeveloped muscles, the main symptom is severe, which leads to death without treatment. The results obtained lead to death. Complications may occur due to hypoxemia and hypercapnia. There is a lung with a right heart that leads to pulmonary treatment. In addition, increased fluid accumulation occurs in predetermined locations. Flat and labored breathing can lead to pneumonia.
A physical examination often provides the first indication of a health condition. The presumptive diagnosis may be supported by a pulmonary function analysis. School medicine therapy focuses on relieving symptoms. In addition to improving the quality of life, it is necessary to achieve a decrease in the mortality rate. Quitting nicotine is indispensable. In addition, mucus and cough suppressants, inhalants, and cortisol medications can make breathing easier. Long-term oxygen therapy is used at an advanced stage.
Causes of the development of pathology in children and adults
Chronic obstructive pulmonary disease is most often diagnosed in people over 40 years of age, but can also be detected in early childhood. The causes of COPD (chronic obstructive pulmonary disease) vary slightly by age.
As a result, the patient cannot breathe in enough oxygen, on the one hand, but, on the other hand, cannot breathe in enough carbon dioxide, which can lead to respiratory depression. It's all about a life threatening form in which breathing is wide and partly very acutely restricted. Oxygen uptake is severely limited by constriction in the bronchi or alveoli.
Therefore, it is very important that the patient learns to deal with his disease. Patient education has six components. The patient accepts his illness, ready to follow necessary therapy For example, inhale daily. The patient is aware of the risk factors that worsen his symptoms and, for example, do without smoking.
- The patient recognizes physical activity, such as.
- The patient knows effective coughing methods.
- The patient knows the light league or attends the light group.
Causes of the development of the disease in childhood
COPD in children can develop at any age and may be provoked by factors such as:

COPD in adolescents and young adults may be due to smoking or low physical activity.
Chronic obstructive pulmonary disease: chronic respiratory diseases, including lung smoking. "Smoking a lung" is a colloquial term for the longer term chronic obstructive pulmonary disease. As a result of recurrent inflammation, thickening of the bronchial walls finally occurs. In addition, spasms of the bronchial muscles can cause further narrowing of the airways.
Schemes and dosing regimens
Chronic obstructive pulmonary disease: increased respiratory distress. Increasingly with frequent and heavy expectoration, especially during the day, especially during physical exertion. Especially in the later stages of the disease, a sudden deterioration, usually caused by additional infections, can lead to life-threatening conditions. specific elasticity. . Chronic obstructive pulmonary disease: immediate smoking, oxygen.
It is noted that young people who are not engaged in physical training are much more likely to show signs of respiratory failure.
Provoking factors in adults
COPD is diagnosed most often in people over 40 years of age. This is due to the following provoking factors, such as:
Timely determination of the cause that causes the development of the disease, and its elimination will help prevent the development of serious complications.
The goal is to reduce disease progression and improve patients' quality of life. Oxygen is needed in acute deterioration and in the later stages of the disease with low levels of oxygen in the blood. Nostalgia massages relieve coughing. . When the smoke stops completely, deterioration of the respiratory function can be prevented. Existing pulmonary hypertension can no longer be relied upon.
Treatment of chronic obstructive disease with herbs
The most common complication is a bacterial infection and: respiratory function deteriorates more and more. The patient may require hospitalization and treatment with antibiotics and inhalations. At the final stage of the disease, gas exchange is so severely disturbed that the patient must either fight or even die from oxygen deficiency.
Symptoms and Diagnosis
How is the disease diagnosed? Symptoms depend on the stage of the disease:

But the diagnosis of COPD is made not only on the basis of the emerging symptoms, its manifestations, especially at an early stage, can be confused with other ailments. Before a final diagnosis is made, differential diagnosis with asthma, tuberculosis.
Chronic lung disease also has a long-term impact on the patient's condition. Over time, the pressure in the pulmonary vessels increases = pulmonary. As a result, the right ventricular chamber is overloaded and cardio exercise occurs. This is accompanied by shortness of breath and an increase in limitation of physical elasticity and quality of life.
At first, respiratory distress occurs only with severe physical stress. In the later stages of the disease, respiratory distress may already occur. This can be countered by early therapy, rehabilitation measures and smokers. Other tests may be needed to detect other lung conditions such as asthma.
For this, the patient is prescribed a number of studies:

Only on the basis of all examination data is the diagnosis of COPD made.
Disease prognosis
It is important to remember that the earlier the disease is detected and treatment is started, the better the prognosis will be. COPD in the early stages of development, if provoking factors are excluded and maintenance therapy is regularly taken, allows the patient to lead an active lifestyle for a long time. Pulmonologists note that the earlier the disease is detected, the better the prognosis.
Good therapy results can only be achieved through constant cooperation between doctor and patient. Avoiding smoking and avoiding smoking as much as possible is effective prevention. Smoking cessation courses can help you quit smoking and help you avoid difficulties after stopping smoking, such as weight gain.
Active treatment of this disease and subsequent therapy lead to an improvement in performance and quality of life. Patient education and rehabilitation courses ensure safety in the treatment of illness in everyday life and travel and increase resilience.
With COPD, the prognosis and life expectancy depend on the stage of the disease:

COPD is serious illness, which violates respiratory function lungs, and only timely diagnosis will help to avoid severe disability.
In patients, a full understanding of one's own illness can greatly contribute to the partnership-based decision-making process in choosing the appropriate treatment procedure and thus significantly contribute to the success of treatment. The practice of decision-making on the basis of partnership allows medical workers and patients work together to find the best treatment for the individual patient. Patients who do their own treatment are much more likely to work for their own health. Good patient information is central to patient participation in treatment decisions.
If coughing is often disturbing and shortness of breath appears during moderate physical exertion, then it is necessary to check the functional state of the lungs, because timely detection and treatment of the disease will help to avoid serious complications that can result in disability, and in severe cases, death.
But, if you have been diagnosed with COPD, then in most cases this is not a reason to prepare for death: timely treatment of exacerbations and elimination of provoking factors will help delay the onset of the severe stage of the disease for several decades.
Phases of the development of the disease
In turn, relatives can help their close relatives or loved ones if they are informed about the illness. Last but not least, interested readers also benefit. The content of this information is based on medical advice and adapted to the needs of medical practice. However, the information contained in this document cannot be substituted for medical advice. Below you will find a brief overview of the sections in which this patient information is shared.
The goal of this information service is to provide readers with high quality content that is understandable without the need for medical expertise. There are no claims to completeness. In all cases, the attending physician can and should be consulted. This patient information cannot be replaced by medical advice, diagnosis or therapy. The two most common types are chronic bronchitis and emphysema.
Modern methods of COPD treatment
CHRONIC OBSTRUCTIVE PULMONARY DISEASE
COPD is characterized by a progressive increase in irreversible obstruction as a result of chronic inflammation induced by pollutants, which is based on gross morphological changes in all lung tissue structures involving cardiovascular systems s and respiratory muscles.
COPD leads to limited physical performance, disability of patients and in some cases death.
What is chronic obstructive pulmonary disease
Your doctor may perform lung function tests or blood tests to help diagnose your condition. Chronic obstructive pulmonary disease refers to lung diseases that cause difficulty in breathing and block the flow of air into the lungs.
Chronic bronchitis is inflammation and narrowing of the bronchi. It also creates excess mucus by blocking airflow. You can develop a chronic cough that occurs to clear mucus from your airways. For bronchitis to be considered chronic, you must have a cough that lasts at least three months out of the year for two years.
The term "COPD", taking into account all stages of the disease, includes chronic obstructive bronchitis, chronic purulent obstructive bronchitis, pulmonary emphysema, pneumosclerosis, pulmonary hypertension, chronic cor pulmonale.
Each of the terms - chronic bronchitis, emphysema, pneumosclerosis, pulmonary hypertension, cor pulmonale - reflects only the peculiarity of the morphological and functional changes that occur in COPD.
Emphysema occurs when the lining of the air sacs is damaged and air pockets form in the lungs. When air is trapped, the lungs slowly increase in size and lose elasticity, making breathing difficult because the lungs cannot fully exhale.
The main reason is prolonged cigarette smoking. Half cigarette smoke Air pollution Long-term exposure to harmful fumes or dust in the workplace. These patients develop emphysema located at the base of the lungs. Cyanosis or blue discoloration of the lips or nails. Fatigue.
- Difficulty breathing Chronic cough, often with excess mucus.
- Recurrent respiratory tract infections.
- Sensitivity.
- Tightness.
The appearance in clinical practice of the term "COPD" is a reflection of the basic law of formal logic - "one phenomenon has one name."
According to the International Classification of Diseases and Causes of Death of the 10th revision, COPD is coded according to the code of the underlying disease that led to the development of COPD - chronic obstructive bronchitis and sometimes bronchial asthma.
Epidemiology. It has been established that the prevalence of COPD in the world among men and women in all age groups is 9.3 and 7.3 per 1000 population, respectively.
For the period from 1990 to 1999. The incidence of COPD among women increased more than among men - by 69% compared to 25%.
These data reflect the changing situation among men and women in the prevalence of the most important risk factor for COPD, tobacco smoking, as well as the increased role of women's exposure to household air pollutants in food preparation and fuel combustion.
COPD is one of the most common diseases in which mortality continues to increase.
According to the US National Institutes of Health, COPD mortality rates are low among people under 45 years of age, but in older age groups it ranks 4-5th, that is, one of the leading causes in the structure of mortality in the United States.
Etiology. COPD is defined by the disease that caused it.
COPD is based on a genetic predisposition, which is realized as a result of prolonged exposure to the bronchial mucosa of factors that have a damaging (toxic) effect.
In addition, several loci of mutated genes associated with the development of COPD have been discovered so far in the human genome.
First of all, this is a deficiency of arantithrypsin, the basis of the body's antiprotease activity and the main inhibitor of neutrophil elastase. In addition to congenital deficiency of a1-antitrypsin, hereditary defects in a1-antichymotrypsin, a2-macroglobulin, vitamin D-binding protein, and cytochrome P4501A1 may be involved in the development and progression of COPD.
Pathogenesis. If we talk about chronic obstructive bronchitis, then the main consequence of the impact of etiological factors is the development of chronic inflammation. The localization of inflammation and the features of triggering factors determine the specifics of the pathological process in COB. Biomarkers of inflammation in COB are neutrophils.
They are predominantly involved in the formation of local antiprotease deficiency, the development of "oxidative stress", play a key role in the chain of processes characteristic of inflammation, leading ultimately to irreversible morphological changes.
An important role in the pathogenesis of the disease is played by impaired mucociliary clearance. The efficiency of mucociliary transport, the most important component of the normal functioning of the airways, depends on the coordination of the action of the ciliated apparatus of the ciliated epithelium, as well as the qualitative and quantitative characteristics of bronchial secretions.
Under the influence of risk factors, the movement of cilia is disrupted up to a complete stop, metaplasia of the epithelium develops with the loss of cells of the ciliated epithelium and an increase in the number of goblet cells. The composition of the bronchial secretion changes, which disrupts the movement of significantly thinned cilia.
This contributes to the occurrence of mucostasis, causing blockade of the small airways. The change in the viscoelastic properties of the bronchial secretion is also accompanied by significant qualitative changes in the composition of the latter: the content of nonspecific components of local immunity in the secretion, which have antiviral and antimicrobial activity - interferon, lactoferin and lysozyme - decreases. Along with this, the content of secretory IgA decreases.
Violations of mucociliary clearance and the phenomenon of local immunodeficiency create optimal conditions for the colonization of microorganisms.
Thick and viscous bronchial mucus with reduced bactericidal potential is a good breeding ground for various microorganisms (viruses, bacteria, fungi).
The whole complex of the listed pathogenetic mechanisms leads to the formation of two main processes characteristic of COB: impaired bronchial patency and the development of centrilobular emphysema.
Bronchial obstruction in COB consists of irreversible and reversible components.
The irreversible component is determined by the destruction of the elastic collagen base of the lungs and fibrosis, changes in the shape and obliteration of the bronchioles. The reversible component is formed due to inflammation, contraction of bronchial smooth muscles and mucus hypersecretion. Ventilation disorders in COB are mainly obstructive, which is manifested by expiratory dyspnea and a decrease in FEV, an indicator that reflects the severity of bronchial obstruction. The progression of the disease, as a mandatory sign of COB, is manifested by an annual decrease in FEV1 by 50 ml or more.
Classification. Experts of the international program "Global Initiative for Chronic Obstructive Lung Disease" (GOLD - Global Strategy for Chronic Obstructive Lung Disease) distinguish the following stages of COPD:
■ Stage I - mild COPD. At this stage, the patient may not notice that his lung function is impaired. Obstructive disorders - the ratio of FEV1 to forced vital capacity of the lungs is less than 70%, FEV1 is more than 80% of the proper values. Usually, but not always, chronic cough and sputum production.
■ Stage II - moderate COPD. This is the stage at which patients apply for medical care due to shortness of breath and exacerbation of the disease. It is characterized by an increase in obstructive disorders (FEV1 is more than 50%, but less than 80% of the due values, the ratio of FEV1 to forced vital capacity is less than 70%). There is an increase in symptoms with shortness of breath that appears with physical activity.
■ Stage III - severe course of COPD. It is characterized by a further increase in airflow limitation (the ratio of FEV1 to forced vital capacity is less than 70%, FEV1 is more than 30%, but less than 50% of the proper values), an increase in shortness of breath, and frequent exacerbations.
■ Stage IV - extremely severe course of COPD. At this stage, the quality of life deteriorates markedly, and exacerbations can be life-threatening. The disease acquires a disabling course. It is characterized by extremely severe bronchial obstruction (the ratio of FEV1 to forced vital capacity is less than 70%, FEV1 is less than 30% of expected values, or FEV1 is less than 50% of proper values in the presence of respiratory failure). Respiratory failure: paO2 less than 8.0 kPa (60 mmHg) or oxygen saturation less than 88% with or without paCO2 greater than 6.0 kPa (45 mmHg). At this stage, cor pulmonale may develop.
The course of the disease. When assessing the nature of the course of the disease, it is important not only to change the clinical picture, but also to determine the dynamics of the fall in bronchial patency. In this case, the determination of the FEV1 parameter - the forced expiratory volume in the first second - is of particular importance. Normally, with age, non-smokers experience a drop in FEV1 by 30 ml per year. In smokers, the decrease in this parameter reaches 45 ml per year. A prognostically unfavorable sign is an annual decrease in FEV1 by 50 ml, which indicates a progressive course of the disease.
Clinic. The main complaint in the relatively early stages of the development of chronic obstructive bronchitis is a productive cough, mainly in the morning. With the progression of the disease and the addition of an obstructive syndrome, more or less constant shortness of breath appears, the cough becomes less productive, paroxysmal, hacking.
Auscultation reveals a wide variety of phenomena: weakened or hard breathing, dry whistling and various wet rales, in the presence of pleural adhesions, a persistent pleural "crack" is heard. Patients with severe disease usually have clinical symptoms emphysema; dry rales, especially on forced exhalation; in the later stages of the disease, weight loss is possible; cyanosis (in its absence, there may be a slight hypoxemia); there is a presence of peripheral edema; swelling of the cervical veins, an increase in the right heart.
Auscultation determines the splitting of the first tone in the pulmonary artery. The appearance of noise in the projection area of the tricuspid valve indicates pulmonary hypertension, although auscultatory symptoms may be masked by severe emphysema.
Signs of an exacerbation of the disease: the appearance of purulent sputum; increase in the amount of sputum; increased shortness of breath; increased wheezing in the lungs; the appearance of heaviness in the chest; fluid retention.
Acute phase reactions of blood are weakly expressed. Erythrocytosis and an associated decrease in ESR may develop.
In sputum, causative agents of exacerbation of COB are detected.
Chest radiographs may show increased and deformed bronchovascular pattern and signs of pulmonary emphysema. The function of external respiration is disturbed according to the obstructive type or mixed with a predominance of obstructive.
Diagnostics. The diagnosis of COPD should be considered in every person who has a cough, excessive sputum production, and/or shortness of breath. It is necessary to take into account the risk factors for the development of the disease in each patient.
In the presence of any of these symptoms, it is necessary to conduct a study of the function of external respiration.
These signs are not diagnostically significant in isolation, but the presence of several of them increases the likelihood of the disease.
Chronic cough and excessive sputum production often long precede ventilation problems leading to dyspnoea.
It is necessary to talk about chronic obstructive bronchitis with the exclusion of other causes of the development of bronchial obstruction syndrome.
Diagnosis criteria - risk factors + productive cough + bronchial obstruction.
Establishing a formal diagnosis of COB entails the next step - determining the degree of obstruction, its reversibility, as well as the severity of respiratory failure.
COB should be suspected in patients with chronic productive cough or exertional dyspnea, the origin of which is unclear, and if there are signs of slow forced expiratory flow.
The basis for the final diagnosis are:
- detection of functional signs of airway obstruction that persists despite intensive treatment using all possible means;
- exclusion of a specific pathology (for example, silicosis, tuberculosis or tumor of the upper respiratory tract) as the cause of these functional disorders.
So, the key symptoms for the diagnosis of COPD.
Chronic cough bothers the patient constantly or periodically; more often observed during the day, less often at night.
Cough is one of the leading symptoms of the disease; its disappearance in COPD may indicate a decrease in the cough reflex, which should be considered as an unfavorable sign.
Chronic sputum production: at the beginning of the disease, the amount of sputum is small. The sputum is mucous in nature and is excreted mainly in the morning.
However, with an exacerbation of the disease, its amount may increase, it becomes more viscous, the color of sputum changes. Shortness of breath: progressive (increases with time), persistent (daily). Increases with exertion and during respiratory infectious diseases.
The action of risk factors in history; smoking and tobacco smoke; industrial dust and chemicals; smoke from household heating appliances and fumes from cooking.
During a clinical examination, an elongated expiratory phase in the respiratory cycle is determined, over the lungs - with percussion a pulmonary sound with a box shade, with auscultation of the lungs - weakened vesicular breathing, scattered dry rales. The diagnosis is confirmed by a study of the function of external respiration.
Determination of forced vital capacity (FVC), forced expiratory volume in the first second (FEV1) and calculation of the FEV / FVC index. Spirometry shows a characteristic decrease in expiratory respiratory flow with a slowdown in forced expiratory flow (decrease in FEV1). Forced expiratory slowing is also clearly seen in the flow-volume curves. VC and fVC are somewhat reduced in patients with severe COB, but closer to normal than the exhalation parameters.
FEV1 is much lower than normal; the FEV1/VC ratio in clinically severe COPD is usually below 70%.
The diagnosis can be considered confirmed only if these disorders persist despite long-term, maximally intensive treatment. An increase in FEV1 of more than 12% after inhalation of bronchodilators indicates a significant reversibility of airway obstruction. It is often noted in patients with COB, but is not pathognomonic for the latter. The absence of such reversibility, when judged by a single test, does not always indicate a fixed obstruction.
Quite often reversibility of obstruction comes to light only after long, most intensive drug treatment. The establishment of a reversible component of bronchial obstruction and its more detailed characterization are carried out during inhalation tests with bronchodilators (anticholinergics and b2-agonists).
The test with berodual allows you to objectively assess both the adrenergic and cholinergic components of the reversibility of bronchial obstruction. In most patients, there is an increase in FEV1 after inhalation of anticholinergic drugs or sympathomimetics.
Bronchial obstruction is considered reversible with an increase in FEV1 by 12% or more after inhalation of pharmaceuticals.
It is recommended to conduct a pharmacological test before prescribing bronchodilatory therapy. At home, for monitoring lung function, it is recommended to determine the peak expiratory flow rate (PEF) using peak flow meters.
The steady progression of the disease is the most important sign of COPD. expressiveness clinical signs in patients with COPD is constantly increasing. To determine the progression of the disease, a repeated determination of FEV1 is used. A decrease in FEV1 by more than 50 ml per year indicates the progression of the disease.
With COB, disturbances in the distribution of ventilation and perfusion occur and manifest themselves in various ways. Excessive ventilation of the physiological dead space indicates the presence in the lungs of areas where it is very high in comparison with the blood flow, i.e., it goes “idle”. Physiological shunting, in contrast, indicates the presence of poorly ventilated but well-perfused alveoli.
In this case, part of the blood coming from the pulmonary arteries to the left heart is not fully oxygenated, which leads to hypoxemia.
In the later stages, general alveolar hypoventilation occurs with hypercapnia exacerbating the hypoxemia caused by physiological shunting.
Chronic hypercapnia is usually well compensated and blood pH is close to normal, except for periods of sharp exacerbation of the disease. X-ray of the chest organs.
Examination of the patient should begin with the production of images in two mutually perpendicular projections, preferably on a film measuring 35x43 cm with an X-ray image intensifier.
Polyprojection radiography allows you to judge the localization and extent of the inflammatory process in the lungs, the condition of the lungs as a whole, the roots of the lungs, pleura, mediastinum and diaphragm. A picture only in a direct projection is allowed for patients who are in a very serious condition. CT scan.
Structural changes in the lung tissue are significantly ahead of irreversible airway obstruction, detected in the study of the function of external respiration and estimated by average indicators of less than 80% of the proper values.
In the zero stage of COPD, using CT, gross changes in the lung tissue are detected. This raises the question of starting the treatment of the disease as early as possible. In addition, CT makes it possible to exclude the presence of lung tumors, the likelihood of which in chronic smokers is much higher than in healthy people. CT can detect widespread congenital malformations in adults: cystic lung, pulmonary hypoplasia, congenital lobar emphysema, bronchogenic cysts, bronchiectasis, as well as structural changes in the lung tissue associated with other past lung diseases that can significantly affect the course of COPD.
In COPD, CT allows examining the anatomical characteristics of the affected bronchi, determining the extent of these lesions in the proximal or distal part of the bronchus; with the help of these methods, bronchial etases are better diagnosed, their localization is clearly established.
With the help of electrocardiography, the state of the myocardium and the presence of signs of hypertrophy and overload of the right ventricle and atrium are assessed.
At laboratory research erythrocyte count may reveal erythrocytosis in patients with chronic hypoxemia.
When determining the leukocyte formula, eosinophilia is sometimes detected, which, as a rule, indicates COB of the asthmatic type.
Sputum examination is useful for determining cellular composition bronchial secretion, although the value of this method is relative. Bacteriological research sputum is necessary to identify the pathogen with signs of a purulent process in the bronchial tree, as well as its sensitivity to antibiotics. Assessment of symptoms.
Rate of progression and severity COPD symptoms depend on the intensity of the impact of etiological factors and their combined action. In typical cases, the disease makes itself felt over the age of 40 years. Cough is the earliest symptom, appearing by 40-50 years of age. By this time, episodes begin to occur during the cold seasons. respiratory infection, not associated initially in one disease.
Subsequently, the cough takes on a daily character, rarely aggravated at night. Cough is usually unproductive; can be paroxysmal in nature and provoked by inhalation of tobacco smoke, weather changes, inhalation of dry cold air and a number of other factors environment.
Sputum is secreted in a small amount, more often in the morning, and has a mucous character. Exacerbations of an infectious nature are manifested by the aggravation of all signs of the disease, the appearance of purulent sputum and an increase in its amount, and sometimes a delay in its release. Sputum has a viscous consistency, often "lumps" of secretion are found in it.
With an exacerbation of the disease, sputum becomes greenish in color, may appear bad smell.
The diagnostic value of an objective examination in COPD is negligible. Physical changes depend on the degree of airway obstruction, the severity of emphysema.
The classic signs of COB are wheezing with a single breath or with forced expiration, indicating a narrowing of the airways. However, these signs do not reflect the severity of the disease, and their absence does not exclude the presence of COB in a patient.
Other signs, such as weakening of breathing, restriction of chest expansion, participation of additional muscles in the act of breathing, central cyanosis, also do not indicate the degree of airway obstruction.
Bronchopulmonary infection - although frequent, but not the only cause of exacerbation.
Along with this, it is possible to develop an exacerbation of the disease due to the increased action of exogenous damaging factors or with inadequate physical activity. In these cases, signs of damage to the respiratory system are less pronounced.
As the disease progresses, the intervals between exacerbations become shorter.
Shortness of breath as the disease progresses can vary from a feeling of lack of air during habitual physical exertion to pronounced manifestations at rest.
Dyspnea felt on exertion occurs on average 10 years after the onset of cough.
It is the reason for most patients to see a doctor and the main cause of disability and anxiety associated with the disease.
As you go down lung function shortness of breath becomes more pronounced. With emphysema, the onset of the disease is possible from it.
This occurs in situations where a person comes into contact with finely dispersed (less than 5 microns) pollutants at work, as well as in hereditary a1-antitrypsin deficiency, leading to the early development of panlobular emphysema.
The Medical Research Council Dyspnea Scale (MRC) is used to quantify the severity of dyspnea.
When formulating the diagnosis of COPD, the severity of the course of the disease is indicated: mild course (stage I), moderate course (stage II), severe course (stage III) and extremely severe course (stage IV), exacerbation or remission of the disease, exacerbation of purulent bronchitis (if any) ; the presence of complications (cor pulmonale, respiratory failure, circulatory failure), indicate risk factors, smoker index.
COPD treatment in a stable state.
1. Bronchodilators occupy a leading place in the complex therapy of COPD. To reduce bronchial obstruction in patients with COPD, short- and long-acting anticholinergic drugs, short- and long-acting b2-agonists, methylxanthines, and their combinations are used.
Bronchodilators are given "on demand" or on a regular basis to prevent or reduce symptoms of COPD.
To prevent the rate of progression of bronchial obstruction, long-term and regular treatment is a priority. M-cholinolytic drugs are considered first-line drugs in the treatment of COPD and their prescription is mandatory for all degrees of severity of the disease.
Regular treatment with long-acting bronchodilators (tiotropium bromide - spiriva, salmeterol, formoterol) is recommended for moderate, severe and very severe COPD.
Patients with moderate, severe or extremely severe COPD are prescribed inhaled M-cholinolytics, long-acting b2-agonists as monotherapy or in combination with prolonged theophyllines. Xanthines are effective in COPD, but due to their potential toxicity, they are second-line drugs. They can be added to regular inhaled bronchodilator therapy for more severe disease.
Anticholinergic drugs(AHP). Inhalation administration of anticholinergic drugs (M-anticholinergics) is advisable for all degrees of severity of the disease. Parasympathetic tone is the leading reversible component of bronchial obstruction in COPD. Therefore, ACPs are the first choice in the treatment of COPD. Short acting anticholinergic drugs.
The best known short-acting AChP is ipratropium bromide, available as a metered-dose aerosol inhaler. Ipratropium bromide inhibits vagus nerve reflexes, being an antagonist of acetylcholine, a parasympathetic mediator nervous system. Dosed at 40 mcg (2 doses) four times a day.
The sensitivity of M-cholinergic receptors of the bronchi does not weaken with age. This is especially important, as it allows the use of anticholinergics in elderly patients with COPD. B
Due to the low absorption through the bronchial mucosa, ipratropium bromide practically does not cause systemic side effects, which allows it to be widely used in patients with cardiovascular diseases.
ACPs do not have a negative effect on the secretion of bronchial mucus and the processes of mucociliary transport.
Short-acting M-cholinolytics have a longer bronchodilator effect compared to short-acting b2-agonists.
Many studies have shown that long-term use Ipratropium bromide is more effective for the treatment of COPD than long-term monotherapy with short-acting β2-agonists.
Long-term use of ipratropium bromide improves the quality of sleep in patients with COPD.
Experts from the American Thoracic Society suggest that ipratropium bromide be used "...for as long as the symptoms of the disease continue to cause discomfort to the patient."
Ipratropium bromide improves the overall quality of life of patients with COPD when used 4 times a day and reduces the number of exacerbations of the disease compared with the use of short-acting b2 ~ agonists.
The use of the inhaled anticholinergic drug ipratropium bromide 4 times a day improves the general condition.
The use of IB as monotherapy or in combination with short-acting β2-agonists reduces the frequency of exacerbations, thereby reducing the cost of treatment.
Long-acting anticholinergics.
A representative of a new generation of AHP is tiotropium bromide (spiriva) in the form of powder capsules for inhalation with a special metered-dose powder inhaler Handi Haler. In one inhalation dose of 0.018 mg of the drug, the peak of action is in 30-45 minutes, the duration of action is 24 hours.
Its only drawback is its relatively high cost.
A significant duration of action of tiotropium bromide, which makes it possible to use it once a day, is ensured by its slow dissociation from M-cholinergic receptors of smooth muscle cells. Long-term bronchodilation (24 hours), recorded after a single inhalation of tiotropium bromide, persists even with its long-term use for 12 months, which is accompanied by an improvement in bronchial patency, regression of respiratory symptoms, and an improvement in the quality of life. With long-term treatment of patients with COPD, the therapeutic superiority of tiotropium bromide over ipratropium bromide and salmeterol has been proven.
2. b2-agonists
short-acting b2 agonists.
In mild COPD, the use of short-acting inhaled bronchodilators "on demand" is recommended. The effect of short-acting b2-agonists (salbutamol, fenoterol) begins within a few minutes, reaching a peak after 15-30 minutes, and lasts for 4-6 hours.
Patients in most cases note relief of breathing immediately after the use of a b2-agonist, which is an undoubted advantage of the drugs.
The bronchodilator effect of b2-agonists is provided by stimulation of b2-receptors of smooth muscle cells.
In addition, due to an increase in the concentration of AMP under the influence of b2-agonists, not only relaxation of the smooth muscles of the bronchi occurs, but also an increase in the beating of the cilia of the epithelium and an improvement in the function of mucociliary transport. The bronchodilating effect is higher, the more distally the predominant violation of bronchial patency is.
After the use of short-acting b2-agonists, patients within a few minutes feel a significant improvement in their condition, the positive effect of which is often overestimated by them.
The regular use of short-acting b2-agonists as monotherapy in COPD is not recommended.
Drugs in this group can cause systemic reactions in the form of transient tremors, agitation, increased blood pressure, which may be of clinical importance in patients with concomitant coronary artery disease and hypertension.
However, when inhalation administration b2-agonists at therapeutic doses, these phenomena are rare.
long-acting b2-agonists (salmeterol and formoterol), regardless of changes in bronchial patency, can improve clinical symptoms and quality of life in patients with COPD, reduce the number of exacerbations.
long-acting b2-agonists reduce bronchial obstruction due to the 12-hour elimination of bronchial smooth muscle constriction. In vitro, the ability of salmeterol to protect the epithelium of the respiratory tract from the damaging effects of bacteria (Haemophilus influenzae) has been shown.
Long-acting b2-agonist salmeterol improves the condition of patients with COPD when used at a dose of 50 mcg twice a day.
Formoterol has a beneficial effect on respiratory function, symptoms and quality of life in patients with COPD.
In addition, salmeterol improves the contractility of the respiratory muscles, reducing respiratory muscle weakness and dysfunction.
Unlike salmeterol, formoterol has a rapid onset of action (after 5-7 minutes).
The duration of action of prolonged b2-agonists reaches 12 hours without loss of effectiveness, which allows us to recommend the latter for regular use in the treatment of COPD.
3. Combinations bronchodilators medicines.
The combination of an inhaled β2-agonist (fast-acting or slow-acting) and AChP is accompanied by an improvement in bronchial patency to a greater extent than with the appointment of any of these drugs as monotherapy.
In moderate and severe COPD, selective b2-agonists are recommended to be prescribed together with M-anticholinergics. Very convenient and less expensive are fixed combinations of drugs in one inhaler (berodual = IB 20 mcg + fenoterol 50 mcg).
The combination of bronchodilators with different mechanisms of action improves efficacy and reduces the risk of side effects compared to increasing the dose of a single drug.
With long-term use (for 90 days or more), IB in combination with b2-agonists does not develop tachyphylaxis.
In recent years, positive experience has begun to accumulate in the combination of anticholinergics with long-acting b2-agonists (for example, with salmeterol).
It has been proven that in order to prevent the progression of bronchial obstruction, long-term and regular treatment with bronchodilators, in particular ACPs and prolonged b2-agonists, is a priority.
4. Long acting theophimines
Methylxanthines are nonselective phosphodiesterase inhibitors.
The bronchodilating effect of theophyllines is inferior to that of b2-agonists and ACPs, but ingestion (prolonged forms) or parenterally (inhaled methylxanthines are not prescribed) causes a number of additional effects that may be useful in a number of patients: reduction of systemic pulmonary hypertension, increased diuresis, stimulation of the central nervous system. system, strengthening the work of the respiratory muscles. Xanthans can be added to regular inhaled bronchodilator therapy for more severe disease with insufficient effectiveness of ACPs and b2-agonists.
In the treatment of COPD, theophylline may be beneficial, but due to its potential toxicity, inhaled bronchodilators are preferred.
All studies that have shown the effectiveness of theophylline in COPD concern long-acting drugs. The use of prolonged forms of theophylline may be indicated for nocturnal manifestations of the disease.
Currently, theophyllines belong to the drugs of the second line, i.e., they are prescribed after ACP and b2-agonists or their combinations.
It is also possible to prescribe theophyllines to those patients who cannot use inhaled delivery vehicles.
According to recent controlled clinical trials, combination therapy with theophylline does not provide additional benefits in the treatment of COPD.
In addition, the use of theophylline in COPD is limited by the risk of adverse reactions.
Tactics of appointment and effectiveness of bronchodilator therapy.
Bronchodilators in patients with COPD can be prescribed both on demand (to reduce the severity of symptoms in a stable state and during exacerbation), and regularly (for prophylactic purposes and to reduce the severity of symptoms).
The dose-response relationship, assessed by the dynamics of FEV, for all classes of bronchodilators is insignificant.
Side effects pharmacologically predictable and dose-dependent. Adverse effects are rare and resolve more rapidly with inhalation than with oral therapy.
In inhalation therapy, special attention should be directed to the effective use of inhalers and patient education in inhalation technique.
When using b2-agonists, tachycardia, arrhythmia, tremor and hypokalemia may develop.
Tachycardia, cardiac arrhythmias and dyspepsia may also occur when taking theophylline, in which doses that provide a bronchodilator effect are close to toxic.
The risk of adverse reactions requires physician attention and monitoring of heart rate, serum potassium levels and ECG analysis, however, there are no standard procedures for assessing the safety of these drugs in clinical practice.
In general, the use of bronchodilators can reduce the severity of dyspnea and other symptoms of COPD, as well as increase exercise tolerance, reduce the frequency of exacerbations of the disease and hospitalizations. On the other hand, regular intake of bronchodilators does not prevent the progression of the disease and does not affect its prognosis.
For mild COPD (stage I) during remission, short-acting bronchodilator therapy is indicated on demand.
In patients with moderate, severe and extremely severe COPD (stages II, III, IV), bronchodilator therapy is indicated with one drug or a combination of bronchodilators.
In some cases, patients with severe and extremely severe COPD (stages III, IV) require regular treatment with high doses of nebulized bronchodilators, especially if they noted a subjective improvement from such treatment, used previously during an exacerbation of the disease.
To clarify the need for inhalation nebulizer therapy, peak flowmetry monitoring is required for 2 weeks and continuation of nebulizer therapy in the presence of a significant improvement in performance.
Bronchodilators are among the most effective symptomatic treatments for COPD.
Methods of delivery of bronchodilators
Exist various ways delivery of bronchodilators in the treatment of COPD: inhalation (ipratropium bromide, tiotropium bromide, salbutamol, fenoterol, formoterol, salmeterol), intravenous (theophylline, salbutamol) and subcutaneous (adrenaline) injections, oral administration (theophylline, salbutamol).
Given that all bronchodilators are capable of causing clinically significant adverse reactions when administered systemically, the inhaled route of delivery is more preferable.
Currently, the domestic market has drugs in the form of a metered-dose aerosol, powder inhalers, solutions for a nebulizer.
When choosing the method of delivery of inhaled bronchodilators, they proceed, first of all, from the patient's ability to correctly use a metered-dose aerosol or other pocket inhaler.
For elderly patients or patients with mental disorders, the use of a metered-dose aerosol with a spencer or a nebulizer is mainly recommended.
Determining factors in the choice of means of delivery are also their availability and cost. Short-acting m-anticholinergics and short-acting b2-agonists are used mainly in the form of metered-dose aerosol inhalers.
To increase the efficiency of drug delivery to the respiratory tract, spacers are used to increase the flow of the drug into the airways. With III and IV COPD stages, especially in respiratory muscle dysfunction syndrome, the best effect is achieved when using nebulizers. allowing to increase the delivery of the drug to the respiratory tract.
When comparing the main means of delivering bronchodilators (metered-dose aerosol inhaler with or without spacer; nebulizer with mouthpiece or face mask; dry-powder metered dose inhaler), their identity was confirmed.
However, the use of nebulizers is preferable in severe patients who, due to severe shortness of breath, cannot perform an adequate inhalation maneuver, which naturally makes it difficult for them to use metered-dose aerosol inhalers and spatial nozzles.
Upon reaching clinical stabilization, patients "return" to the usual means of delivery (metered-dose aerosols or powder inhalers).
Glucocorticosteroids in stable COPD
The therapeutic effect of corticosteroids in COPD is much less pronounced than in asthma, so their use in COPD is limited to certain indications. Inhaled corticosteroids (IGCS) are prescribed in addition to bronchodilator therapy - in patients with FEVR<50% от должной (стадия III: тяжелая ХОБЛ и стадия IV: крайне тяжелая ХОБЛ) и повторяющимися обострениями (3 раза и более за последние три года).
Regular treatment with ICS is indicated for patients with severe and extremely severe disease with annual or more frequent exacerbations over the past three years.
To establish the feasibility of the systematic use of ICS, it is recommended to conduct trial therapy with systemic corticosteroids at a dose of 0.4-0.6 mg/kg/day orally (according to prednisolone) for 2 weeks.
Long-term use of systemic corticosteroids (more than 2 weeks) with a stable course of COPD is not recommended due to the high risk of adverse events.
The effect of steroids should complement the effects of permanent bronchodilator therapy.
Monotherapy with ICS is unacceptable for patients with COPD.
Corticosteroids are preferably administered in the form of metered-dose aerosols.
Unfortunately, even inhaled long-term use of corticosteroids does not reduce the rate of annual decrease in FEV in patients with COPD.
The combination of ICS and long-acting β2-agonists is more effective in the treatment of COPD than the use of individual components.
This combination demonstrates a synergism of action and allows you to influence the pathophysiological components of COPD: bronchial obstruction, inflammation and structural changes in the airways, mucociliary dysfunction.
The combination of long-acting β2-agonists and ICS results in a more advantageous risk/benefit ratio compared to the individual components.
The combination of salmeterol/fluticasone propionate (seretide) has the potential to increase survival in patients with COPD.
Each dose of Seretide (two breaths for a metered dose inhaler) contains 50 micrograms of salmeterol xinafoate in combination with 100 micrograms of fluticasone propionate, or 250 micrograms or 500 micrograms of fluticasone propionate.
It is advisable to use a fixed combination of formoterol and budesonide (symbicort) in patients with moderate to severe COPD compared with the separate use of each of these drugs.
Other medicines
Vaccines. In order to prevent exacerbation of COPD during epidemic outbreaks of influenza, vaccines containing killed or inactivated viruses are recommended for use, administered once in October-first half of November annually. Influenza vaccine can reduce the severity and mortality in patients with COPD by 50%.
A pneumococcal vaccine containing 23 virulent serotypes is also used, but data on its effectiveness in COPD are insufficient.
However, according to the Committee of Advisors on Immunization Practices, patients with COPD are at high risk of developing pneumococcal disease and are included in the target group for vaccination. Preferably polyvalent bacterial vaccines administered orally (ribomunil, bronchomunal, bronchovacom).
Antibacterial drugs. According to the current point of view, antibiotics for the prevention of exacerbations of COPD are not prescribed.
An exception is an exacerbation of COB with the appearance of purulent sputum (appearance or intensification of "purulence") along with an increase in its amount, as well as signs of respiratory failure.
It must be borne in mind that the degree of eradication of etiologically significant microorganisms determines the duration of remission and the timing of the subsequent relapse.
When choosing the optimal antibiotic for a given patient, one should focus on the spectrum of the main pathogens, the severity of exacerbation, the likelihood of regional resistance, the safety of the antibiotic, the convenience of its use, and cost indicators.
First-line drugs in patients with non-severe COB exacerbations are amoxiclav/clavulanic acid or its unprotected form, amoxicillin. Eradication of pathogens of respiratory tract infections allows you to break the vicious circle of the course of the disease.
In the majority of patients with COB, macrolides are effective despite the resistance of S. pneumoniae registered to them and the low natural sensitivity of H. influenzae.
This effect may be partly due to the anti-inflammatory activity of macrolides.
Among macrolides, mainly azithromycin and clarithromycin are used.
An alternative to protected penicillins can be respiratory fluoroquinolones (sparfloxacin, moxifloxacin, levofloxacin), which have a wide spectrum of antimicrobial activity against gram-positive and gram-negative microorganisms, penicillin-resistant strains of S. pneumoniae and H. influenzae.
Respiratory fluoroquinolones are able to create a high concentration in the bronchial contents, have almost complete bioavailability when taken orally. In order to ensure high compliance of patients, the prescribed antibiotic should be taken orally 1-2 times a day and for at least 5, preferably 7 days, which meets the modern requirements of antibiotic therapy for COB exacerbation.
Mucolytic agents
Mucolytics (mucokinetics, mucoregulators) are indicated for a limited group of patients with stable COPD in the presence of viscous sputum. The effectiveness of mucolytics in the treatment of COPD is low, although some patients with viscous sputum may improve.
At present, based on existing evidence, the widespread use of these drugs cannot be recommended in stable COPD.
With COB, ambroxol (lazolvan), acetylcysteine are most effective. The previously practiced use of proteolytic enzymes as mucolytics is unacceptable.
Long-term use of the mucolytic N-acetylcysteine (NAC), which simultaneously has antioxidant activity, seems promising for the prevention of COPD exacerbation.
Taking NAC (fluimucil) for 3-6 months at a dose of 600 mg/day is accompanied by a significant decrease in the frequency and duration of COPD exacerbations.
Other pharmacological agents. Prescribing psychotropic drugs to elderly patients with COPD for the treatment of depression, anxiety, insomnia should be carried out with caution due to their inhibitory effect on the respiratory center.
In severe COPD with the development of LS, there is a need for cardiovascular therapy,
In such cases, treatment may include ACE inhibitors, CCBs, diuretics, and possibly digoxin.
Appointment of adrenergic blockers is contraindicated.
Non-drug treatment with stable COPD.
1. Oxygen therapy.
2. Surgical treatment (see below in the section "Treatment of emphysema").
3. Rehabilitation.
Oxygen therapy. The main cause of death in COPD patients is DN. Correction of hypoxemia with oxygen is the most pathophysiologically substantiated method for the treatment of DN.
The use of oxygen in patients with chronic hypoxemia must be constant, long-term, and usually done at home, so this form of therapy is called long-term oxygen therapy (LOT).
VCT is currently the only therapy that can reduce mortality in patients with COPD.
Other beneficial physiological and clinical effects of VCT include:
reverse development and prevention of progression of pulmonary hypertension;
reduction of shortness of breath and increased tolerance to physical activity;
decrease in hematocrit;
improving the function and metabolism of the respiratory muscles;
improvement of the neuropsychological status of patients;
reduction in the frequency of hospitalizations of patients.
Indications for long-term oxygen therapy. Long-term oxygen therapy is indicated for patients with severe COPD.
Before prescribing VCT to patients, it is also necessary to make sure that the possibilities of drug therapy have been exhausted and that the maximum possible therapy does not lead to an increase in O2 above the borderline values. It has been proven that long-term (more than 15 hours per day) oxygen therapy increases the life expectancy of patients with DN.
The goal of long-term oxygen therapy is to increase PaO2 to at least 60 mm Hg. Art. at rest and/or SaO2 not less than 90%. It is considered optimal to maintain PaO, within 60-65 mm Hg. Art.
Continuous oxygen therapy is indicated for:
- PaO2< 55 мм рт. ст. или SaО2 < 88% в покое;
- PaO2 56-59 mm Hg. Art. or SaO2 = 89% in the presence of CHLS and/or erythrocytosis (Ht > 55%).
"Situational" oxygen therapy is indicated for:
- decrease in PaO2< 55 мм рт. ст. или Sa02 < 88% при физической нагрузке; - снижении РаО2 < 55 мм рт. ст. или Sa02 < 88% во время сна.
VCT is not indicated for patients with moderate hypoxemia (PaO2 > 60 mm Hg).
The parameters of gas exchange, on which indications for VCT are based, should only be assessed during the stable state of patients, i.e. 3-4 weeks after an exacerbation of COPD, since this is the time required for the restoration of gas exchange and oxygen transport after a period of acute respiratory failure ( ODN).
Rehabilitation. It is prescribed in all phases of COPD. Depending on the severity, phase of the disease and the degree of compensation of the respiratory and cardiovascular systems, the attending physician determines individual program rehabilitation for each patient, which includes a regimen, exercise therapy, physiotherapy, spa treatment. Therapeutic breathing exercises are recommended for COPD patients even in the presence of severe obstruction.
An individually tailored program leads to an improvement in the patient's quality of life. Perhaps the use of transcutaneous electrical stimulation of the diaphragm. To give up smoking.
Smoking cessation is an extremely important intervention that improves the prognosis of the disease.
It should take the first place in the treatment of this pathology. Smoking cessation reduces the degree and rate of fall in FEV1
The use of auxiliary artificial lung ventilation can be considered with an increase in pCO2 and a decrease in blood pH in the absence of the effect of the above therapy.
Indications for hospitalization: ineffective treatment on an outpatient basis; increase in symptoms of obstruction, inability to move around the room (for a previously mobile person); increase in shortness of breath during meals and during sleep; progressive hypoxemia; the occurrence and / or increase of hypercapnia; the presence of concomitant pulmonary and extrapulmonary diseases; occurrence and progression of symptoms of "cor pulmonale" and its decompensation; mental disorders.
Treatment in a hospital
1. Oxygen therapy. In the presence of a severe exacerbation of the disease and severe respiratory failure, continuous oxygen therapy is indicated.
2. Bronchodilator therapy is carried out with the same drugs as in outpatient treatment. Spraying b2-agonists and anticholinergics is recommended using a nebulizer, inhaling every 4-6 hours.
With insufficient efficiency, the frequency of inhalations can be increased. Combinations of drugs are recommended.
When therapy through a nebulizer, it can be done within 24-48 hours.
In the future, bronchodilators are prescribed in the form of a metered aerosol or dry powder. If inhalation therapy is insufficient, intravenous administration of methylxanthines (eufillin, aminophylline, etc.) is prescribed at a rate of 0.5 mg/kg/h.
3. Antibacterial therapy is prescribed if there are the same indications that were taken into account at the outpatient stage of treatment. With the ineffectiveness of primary antibiotic therapy, the selection of an antibiotic is carried out taking into account the sensitivity of the patient's sputum flora to antibacterial drugs.
4. Indications for prescribing and prescribing regimens for glucocorticoid hormones are the same as at the outpatient stage of treatment. In severe cases of the disease, intravenous administration of corticosteroids is recommended.
5. In the presence of edema, diuretics are prescribed.
6. In case of severe exacerbation of the disease, the appointment of heparin is recommended.
7. Auxiliary artificial lung ventilation is used in the absence of a positive effect from the above therapy, with an increase in pCO2 and a drop in pH.
Non-drug methods of treatment are used, first of all, in order to facilitate sputum production, especially if the patient is treated with expectorants, plentiful alkaline drinking.
Positional drainage - coughing up sputum with a deep forced expiration in a position that is optimal for sputum discharge. Coughing improves with the application of vibration massage.
Forecast
The outcome of COPD is the development of chronic cor pulmonale and pulmonary heart failure.
Prognostically unfavorable factors are advanced age, severe bronchial obstruction (in terms of FEV1), the severity of hypoxemia, and the presence of hypercapnia.
The death of patients usually occurs from complications such as acute respiratory failure, cor pulmonale decompensation, severe pneumonia, pneumothorax, and cardiac arrhythmias.
